Takeaway: There are a number of COVID-19 testing options out there. These COVID-19 Testing FAQs will help you make more informed decisions so you can mitigate risk and protect your workforce.
The COVID-19 (SARS-CoV-2) pandemic has changed occupational health and safety on a global scale. With vaccination rates on the rise, there is some light at the end of the tunnel. However we are not yet out of the weeds, and employers still face an immense amount of pressure to keep their workforces safe and healthy.
This article presents some COVID-19 testing FAQs (Frequently Asked Questions) and definitions to help you better understand the types of risk mitigation tools currently available.
What is COVID-19 and what signs/symptoms should I look out for?
COVID-19 is a disease caused by a new strain of coronavirus. ‘CO’ stands for corona, ‘VI’ for virus, and ‘D’ for disease. Formerly, this disease was referred to as ‘2019 novel coronavirus’ or ‘2019-nCoV.’ The COVID-19 virus is a new virus linked to the same family of viruses as Severe Acute Respiratory Syndrome (SARS) and some types of common cold.
Some of the most common signs/symptoms of COVID-19 infection include:
- Fever (80-88% of cases)
- Dry cough (63-69% of cases)
- Loss of appetite (39-84% of cases)
- Fatigue (38-46% of cases)
- Sputum (phlegm) production (33-42% of cases)
- Chest pain or pressure (28-36% of cases)
- Shortness of breath (19-25% of cases)
- Muscle and joint pain (15-33% of cases)
For more information, check out the ACOEM’s (American College of Occupational and Environmental Medicine) COVID-19 Information Guide.
Less common symptoms include:
- Sore throat (12-14% of cases)
- Headaches (11-15% of cases)
- Chills (6-11% of cases)
- Nausea/vomiting (5-10% of cases)
- Diarrhea (4-29% of cases)
- Nasal congestion (4-5% of cases)
- Abdominal pain (4% of cases)
- Pink eye (1% of cases)
Loss of smell and/or taste has also been identified as important symptoms to watch out for in those with moderate to severe cases of COVID-19.
What are the different testing options for COVID-19?
There are a number of different testing options for COVID-19, including:
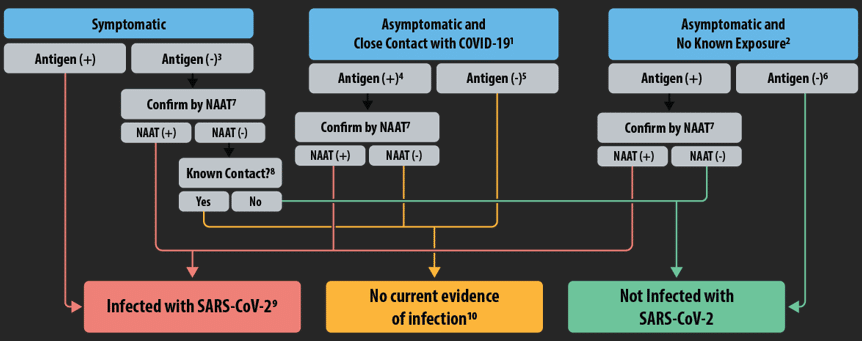
- PCR (Polymerase Chain Reaction) Testing. A PCR test (also known as NAAT or Nucleic Acid Amplification Test) serves as the baseline criterion for identifying genetic material anomalies pointing to an infection of a virus. Recently, this is often in reference to SARS-CoV-2, a form of coronavirus hosting the COVID-19 strain. For individuals experiencing recent symptoms of COVID-19 or having been in close contact with an infected individual within a fifteen-minute interval, a PCR test is recommended. This test is considered to be the gold standard for COVID-19 diagnosis. Read the full definition.
- Antigen Testing. An antigen test is a clinical procedure involving tissue swab fluid samples of the mucus lining from the nasal/nasopharyngeal cavities, targeting the presence of specific proteins in the sample, which indicate current COVID-19 infection in the system. Antigens are compounds that trigger an immune system response through the release of antibodies. Read the full definition.
- Antibody Testing. An antibody test is a clinical procedure administered to individuals following a complete recovery from the COV1D-19 viral strain, noted by a cumulative buildup of antibodies via immune system response against invading antigens. A laboratory technician will draw a sample via finger prick or blood draw from the arm to determine if an individual meets the qualifying criteria after a fourteen-day lapse, allowing for sufficient antibody development. Read the full definition.
The World Health Organization has a number of resources available online to help individuals better understand the test types available. Check out this podcast to learn more from Dr. Hanan Balkhy (Assistant Director of Antimicrobial Resistance at the World Health Organization).
What are the risk mitigation strategies employers are using to prevent COVID-19 transmission in their workforce?
SureHire’s clients are currently using a range of risk mitigation strategies to protect their workforce and minimize the risk of COVID-19 transmission.
Pre-Access Antigen Testing
Rapid antigen tests can help control the spread of disease by offering quick results turnaround. The test provides a qualitative “yes/no” answer on the presence of the pathogen in the patient sample. Within minutes of taking a test, a patient can self-quarantine, effectively eliminating the need to wait for PCR test results from a lab. This quick results turnaround makes risk prevention actionable in real-time.
A test administrator will complete the test by having the participant place a swab into the back of their nose to collect mucous. Next, the administrator will place the sample in a tube and the sample will be analyzed by our Point-of-Care device. Finally, after approximately 15 minutes, the device will notify the administrator whether the participant is positive or negative for COVID-19. A positive test indicates that the individual is positive for active infection of COVID-19.

This test is not diagnostic and a negative result does not mean the individual does not have COVID-19. Antigen testing cannot be used as the sole criteria for determining treatment or for management decisions. Negative results must be used in conjunction with symptom observations, the individual’s health history as well as other pertinent clinical findings.
Screening Questionnaires
Many screening questionnaires aim to identify symptoms of COVID-19 or situations in which an individual may have been exposed to COVID-19 (for example, non-essential travel outside of one’s country of residence). However, there are many pre-existing conditions (such as seasonal allergies, asthma, etc.) that can mimic the symptoms of COVID-19, which can result in employees being unnecessarily sent to self-isolate.
SureHire has developed a screening questionnaire program that not only helps identify symptoms of concern but also arms employers with data regarding symptoms of pre-existing health conditions, so they can make more informed decisions about the health and safety of everyone on the job. Data does not reveal the type of pre-existing condition an employee has. Instead, it simply shows employers that a pre-existing condition is present and may present symptoms similar to COVID-19.
Temperature Screening
Temperature Screening allows you to mitigate risk by checking for fever (a critical symptom of COVID-19). By recording your employees’ temperature at the start of each shift, employers can get an instantaneous result and compare it to the 38°C cut-off level. While readings do not correlate with COVID-19 diagnosis specifically
(as other medical conditions can also present with fever), they do provide valuable, objective data to help you limit the risk of worker exposure and transmission. Temperature readings using FDA-approved devices also ensure accurate results and easy implementation on any worksite.
How can these tools be effectively integrated into my COVID-19 safe-work protocols?
There are a number of ways you can integrate COVID-19 transmission prevention tools into your safe work protocol:
- After being flagged on a daily screening questionnaire. (Learn about our Health Risk Assessment (HRA) Program),
- After being flagged during routine temperature checks. (Learn about our Temperature Screening services, powered by NaviSure.),
- Before gaining access to a remote worksite (e.g. before going to the airport or travelling to the site),
- On a regularly occurring schedule (e.g. at the start of each week),
- Before an event (e.g. conference) (Note: remember to review your provincial or territorial guidelines on events & social gatherings), or
- As a precaution before hiring a new employee.
Get more information and guidance on safe-work protocols and COVID-19 transmission risk prevention.

Learn more about SureHire’s COVID-19 Support Services and contact us today to inquire.